TMJ vs. TMD
If you’re grappling with jaw pain that interferes with basic functions like yawning, speaking, chewing, or swallowing, you might be contending with temporomandibular disorder (TMD). TMD arises from issues with the temporomandibular joints (TMJ) in the jaw, yet many individuals experiencing this discomfort aren’t aware of the distinction between TMJ and TMD. Here’s the breakdown:
What is TMJ?
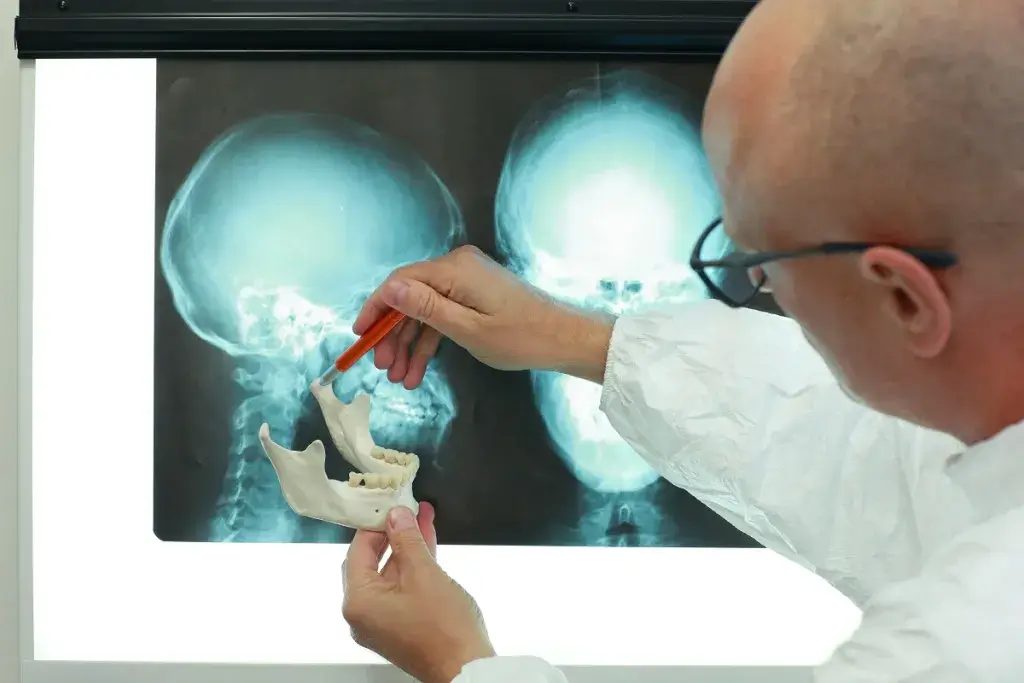
TMJ refers to the temporomandibular joint, a pivotal connection linking the jawbone to the skull via the temporal bone. Serving as both a sliding and hinge joint, the TMJ facilitates mouth opening, speech, and chewing. Although resilient, the TMJ can incur damage, inflammation, or irritation, resulting in discomfort or pain during basic oral activities.
What is TMD?
TMD, short for temporomandibular joint disorder, encompasses any dysfunction affecting the TMJ. This disorder may involve the ligaments, discs, bones, and muscles surrounding the TMJ. Misalignment of the joint can lead to pain, inflammation, or restricted jaw movement. TMD typically affects individuals between 20-40 years old and is more prevalent in females.
Causes of TMD:
TMD’s etiology is multifaceted, making pinpointing a specific cause challenging. Contributing factors often involve issues with the TMJ, jaw, or adjacent muscles. Causes may include injury to TMJ muscles, misalignment of teeth or jaw, arthritis, dislocation of the joint cushion, or teeth clenching or grinding.
Symptoms of TMD:
TMD manifests through a spectrum of symptoms, ranging from temporary discomfort to chronic pain. Symptoms can overlap with other medical conditions, making a dental diagnosis essential. Signs may include earaches, jaw dislocation, headaches, dental occlusion issues, facial swelling, or clicking sounds in the jaw joint.
Diagnosis and Treatment:
Your dentist can diagnose TMD and tailor treatment to your specific needs, considering factors such as medical history and overall health. Treatment options may encompass stress management techniques, prescription medication, physical therapy, behavior modification, dietary adjustments, or dental appliances like mouthguards. In severe cases, surgical intervention may be necessary.
Follow-Up Care:
Promptly seek dental evaluation if you experience jaw pain. Your dentist can recommend suitable treatment based on your unique circumstances, potentially incorporating corrective measures like bite adjustment or dental restorations. Customized solutions aim to mitigate discomfort and restore oral function.
If you’re grappling with jaw discomfort or suspect TMD, consulting your dentist is paramount. Effective management can alleviate symptoms and improve your quality of life.
